Diabetes
Looking After Your Feet
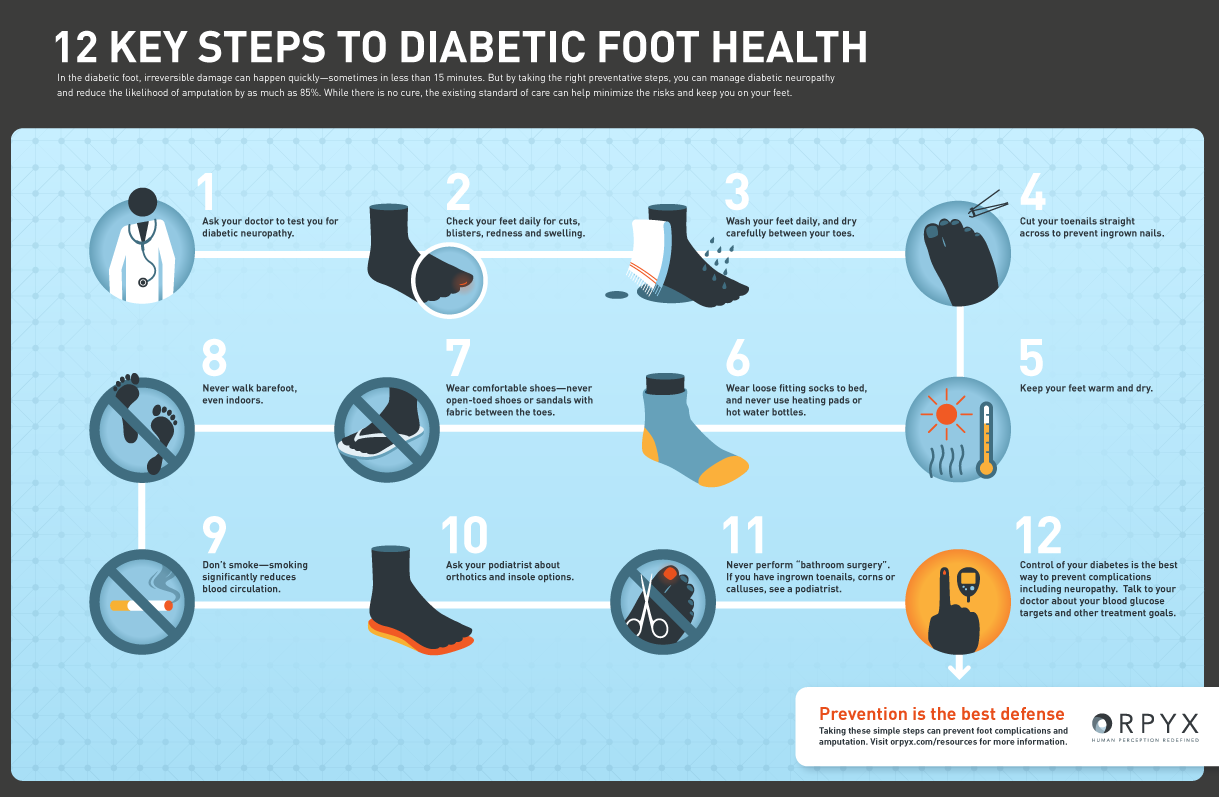
Foot problems are one of the common complications of diabetes and are caused by nerve damage (neuropathy) or damage to blood vessels in the feet and legs.
Podiatrists are clinicians who treat a vast array of foot and lower limb conditions.
Podiatry is about prevention
Prevention of pain, falls, foot ulceration and lower limb amputation.
Around 10% of people with diabetes will have a diabetic foot ulcer at some time in their lives – this is around 4000,000 people
130 amputations take place each week in the UK, 80% of which are preceded by a diabetic foot ulcer.
Minor amputations, such as toes, are increasing. (National Audit Office report 2015)
Podiatrists give their patients an increased quality of life through a service which can help to bring about improved mobility and the ability to exercise more readily. The service is also capable of generating savings for the taxpayer by reducing the need for amputations arising from diabetic foot problems.
Diabetic Foot Problem: Prevention and Management
The key recommendations from NICE guidance
- Everyone with diabetes should be informed of their level of risk of developing foot ulcers and supplied with advice about basic foot care, footwear, blood glucose management, signs of infection and who to contact if a foot emergency occurs.
- Children under 12, their family and carers should be advised on good daily care, warning signs of infection and who to contact if they have concerns. Those aged 12-17 should have their feet screened annually or whenever a problem occurs.
Damage to Nerves and Blood Vessels
Damage to Nerves
From early diagnosis of Diabetes, most people should be told to look after their feet because of the risks that long-term diabetes or poorly controlled diabetes can cause nerve damage.
Symptoms of Neuropathy affecting the feet
- Tingling or buzzing in the feet (paraphasia) which is often worse at night making sleeping difficult.
- Loss of temperature perception the feet are less sensitive to heat and cold
- Exaggerated sensitivity in the skin (called hyperesthesia) An unpleasant sensitivity to skin stimulation, just wearing socks or tights can be very irritating to the skin.
Damage to Blood Vessels
In addition to neuropathy, people with Diabetes can develop foot problems because of damage to blood vessels in the feet and legs. This may mean that less blood gets to the skin muscles and tissues. A poor blood supply to the feet means that any injuries will not heal as quickly as expected.
Changes to the blood supply can cause the following symptoms :
- Cramp in the calves
- Shiny smooth skin
- Loss of hair on the feet and legs
- Thickened toenails
- Cold pale feet
- Change in the color of the skin of the feet
- Wounds or sores
- Pain in your feet, especially when you put them up, such as going to bed, which improves when you put them down. This is a condition called Limb Ischaemia which is a severe obstruction of the arteries which markedly reduces blood flow to the feet and has progressed to the point of severe pain and even skin ulcers and sores. The pain caused by this can wake up an individual at night.
Looking After Your Feet
Check your feet
Once diagnosed with Diabetes you should check your feet every day, even if they look healthy, and your feet should be checked regularly by health professionals.
- Choose when and where you are going to check your feet each day, for instance. it could be when you get up in the morning in the bedroom or after a shower in the bathroom.
- Try to check your feet at the same time as this helps you to remember.
There are some areas of the feet where the skin is more at risk:
- The balls of the feet. You can use a mirror if you can’t manage to look at the soles of your feet.
- Areas where the bones may stick out, such as bunions or hammer toes.
- Places where shoes or socks may rub.
The Changes you are looking for
- Swelling
- Redness or any changes in the color of the skin, for example, pale or bruised skin, cuts or blisters.
- Pain
- Fluid coming from a wound.
Wash Your Feet
- You should wash your feet daily in warm, soapy water.
- Don’t soak your feet too long in the bath as this can cause them to be easily damaged.
- Dry your feet well but gently, especially between the toes to prevent infections, such as athlete’s foot, and avoid sawing the towel between the toes.
Use A Moisturiser
Use a moisturizer after you have dried your feet to keep the skin on your feet supple.
Do not use between the toes because it will make the skin there too moist
If you use talc, only a small amount to avoid it clogging up and increasing the risk of infection.9
Advice on cutting your toenails
If you have been advised by your consultant or GP not to cut your toenails yourself, then you should see a Podiatrist.
- Follow the shape of the toe when cutting
- Leave no sharp edges
- Nails are for protection so do not cut them too short
- Never cut down the sides
- If you have in-growing toenails or you suspect a nail infection Don’t treat it yourself, see a Podiatrist.
The Golden Rules For Looking After Your Feet
- Never go barefoot
- Wear good fitting shoes
- Break in new shoes gradually and make sure they don’t rub
- Keep your feet dry especially between the toes
For more information or to book a consultation contact us.

